(Sacramento, CA)—The California Association of Nurse Anesthesiology(CANA) is proud to announce the success of the inaugural Western Summit for Nurse Anesthesiology, hosted by CANA in collaboration with Western AANA State Associations. Held in Las Vegas, Nevada from October 3-5, 2025, the Summit convened nearly 1,000 attendees, including Certified Registered Nurse Anesthetists (CRNAs), Nurse Anesthesia Residents (NARs), and Registered Nurses (RNs) from 13 participating state associations: Alaska, Arizona, California, Colorado, Hawaii, Idaho, Montana, Nevada, New Mexico, Oregon, Utah, Washington, and Wyoming.
“The Western Summit showcased the strength and unity of nurse anesthesiologists across the western region,” said Emily Francke, MSN, CRNA, outgoing Board President, CANA. “This collaboration reflects our shared commitment to advancing anesthesia care, supporting professional growth, and ensuring patients throughout our states have access to safe, high-quality anesthesia services.”
Through a robust lineup of educational sessions, hands-on workshops, and breakout discussions, attendees explored emerging issues in anesthesia practice, leadership, and patient care, including innovations in anesthesia delivery, non-opioid pain management, workforce development, and technology-driven practice models. Breakout sessions for RNs interested in pursuing nurse anesthesiology careers underscored the profession’s commitment to fostering the next generation of anesthesia providers.
In addition to the educational program, CANA held its annual members meeting to swear in its newly elected Board of Directors and present several awards in recognition of outstanding leadership and contributions to the nurse anesthesiology profession, including:
- Champion for Nurse Anesthesiology Award, presented to Assemblymember Heath Flora (R-Ripon) for his tireless work related to AB 876
- Lifetime Achievement Award,presented to Karyn Karp, MS, CRNA
- Joyce Kelly Education Award, presented to Sassoon Elisha, EdD, APRN, CRNA, FAANA, FAAN
- Medal of Commendation for CRNA Insight, presented to Jacob Schonau-Taylor, MSN, CRNA for his Educational Program for RNs
- Medal of Commendations for their work on AB 876, presented to:
- Emily Francke, MSN, CRNA; Sandra Bordi, DNP, CRNA, FAANA; Elizabeth Bamgbose, PhD, CRNA, FAANA; Kristen Roman, DNAP, CRNA; Thomas Bachtler, DNP, CRNA, CENP; Melanie Rowe, MSN, CRNA
- Katherine Bowles, Fennemore; Kaitlin Perry, Perry Communications Group; Justin Fanslau, Fanslau Government Affairs; Monica Miller, Sacramento Advisors
“We were proud to recognize Assemblymember Flora for his steadfast support of CRNAs and his leadership in expanding access to timely, high-quality anesthesia care for all Californians,” said Kristen Roman, DNAP, CRNA, 2026 Board President, CANA. “He has been instrumental in advancing legislative solutions that reflect the expertise and essential role of CRNAs across our state.”
Adding to a year of significant accomplishments, CANA was also recognized earlier in the year by the American Association of Nurse Anesthesiology (AANA). The 2024-2025 AANA Communications Committee selected CANA as a recipient of the 2025 AANA Public Relations Recognition Award for Best Promotional Effort for National CRNA Week.
Building on CANA’s commitment to closing care gaps and meeting patients where they are, CANA is holding a rural health symposium in early 2026. The event will spotlight CRNAs’ critical role in rural landscapes and strategies to mitigate California’s health care workforce shortage to ensure all Californians have access to high-quality, safe, and timely surgical care.
About CANA
The California Association of Nurse Anesthesiology (CANA) represents CRNAs across the state. Since 1931, CANA has provided leadership, advocacy, and education to advance patient safety and support the nurse anesthesia profession. Learn more at www.canainc.org.
(Sacramento, CA)—The California Association of Nurse Anesthesiology(CANA) is proud to announce the success of the inaugural Western Summit for Nurse Anesthesiology, hosted by CANA in collaboration with Western AANA State Associations. Held in Las Vegas, Nevada from October 3-5, 2025, the Summit convened nearly 1,000 attendees, including Certified Registered Nurse Anesthetists (CRNAs), Nurse Anesthesia Residents (NARs), and Registered Nurses (RNs) from 13 participating state associations: Alaska, Arizona, California, Colorado, Hawaii, Idaho, Montana, Nevada, New Mexico, Oregon, Utah, Washington, and Wyoming.
“The Western Summit showcased the strength and unity of nurse anesthesiologists across the western region,” said Emily Francke, MSN, CRNA, outgoing Board President, CANA. “This collaboration reflects our shared commitment to advancing anesthesia care, supporting professional growth, and ensuring patients throughout our states have access to safe, high-quality anesthesia services.”
Through a robust lineup of educational sessions, hands-on workshops, and breakout discussions, attendees explored emerging issues in anesthesia practice, leadership, and patient care, including innovations in anesthesia delivery, non-opioid pain management, workforce development, and technology-driven practice models. Breakout sessions for RNs interested in pursuing nurse anesthesiology careers underscored the profession’s commitment to fostering the next generation of anesthesia providers.
In addition to the educational program, CANA held its annual members meeting to swear in its newly elected Board of Directors and present several awards in recognition of outstanding leadership and contributions to the nurse anesthesiology profession, including:
- Champion for Nurse Anesthesiology Award, presented to Assemblymember Heath Flora (R-Ripon) for his tireless work related to AB 876
- Lifetime Achievement Award,presented to Karyn Karp, MS, CRNA
- Joyce Kelly Education Award, presented to Sassoon Elisha, EdD, APRN, CRNA, FAANA, FAAN
- Medal of Commendation for CRNA Insight, presented to Jacob Schonau-Taylor, MSN, CRNA for his Educational Program for RNs
- Medal of Commendations for their work on AB 876, presented to:
- Emily Francke, MSN, CRNA; Sandra Bordi, DNP, CRNA, FAANA; Elizabeth Bamgbose, PhD, CRNA, FAANA; Kristen Roman, DNAP, CRNA; Thomas Bachtler, DNP, CRNA, CENP; Melanie Rowe, MSN, CRNA
- Katherine Bowles, Fennemore; Kaitlin Perry, Perry Communications Group; Justin Fanslau, Fanslau Government Affairs; Monica Miller, Sacramento Advisors
“We were proud to recognize Assemblymember Flora for his steadfast support of CRNAs and his leadership in expanding access to timely, high-quality anesthesia care for all Californians,” said Kristen Roman, DNAP, CRNA, 2026 Board President, CANA. “He has been instrumental in advancing legislative solutions that reflect the expertise and essential role of CRNAs across our state.”
Adding to a year of significant accomplishments, CANA was also recognized earlier in the year by the American Association of Nurse Anesthesiology (AANA). The 2024-2025 AANA Communications Committee selected CANA as a recipient of the 2025 AANA Public Relations Recognition Award for Best Promotional Effort for National CRNA Week.
Building on CANA’s commitment to closing care gaps and meeting patients where they are, CANA is holding a rural health symposium in early 2026. The event will spotlight CRNAs’ critical role in rural landscapes and strategies to mitigate California’s health care workforce shortage to ensure all Californians have access to high-quality, safe, and timely surgical care.
About CANA
The California Association of Nurse Anesthesiology (CANA) represents CRNAs across the state. Since 1931, CANA has provided leadership, advocacy, and education to advance patient safety and support the nurse anesthesia profession. Learn more at www.canainc.org.
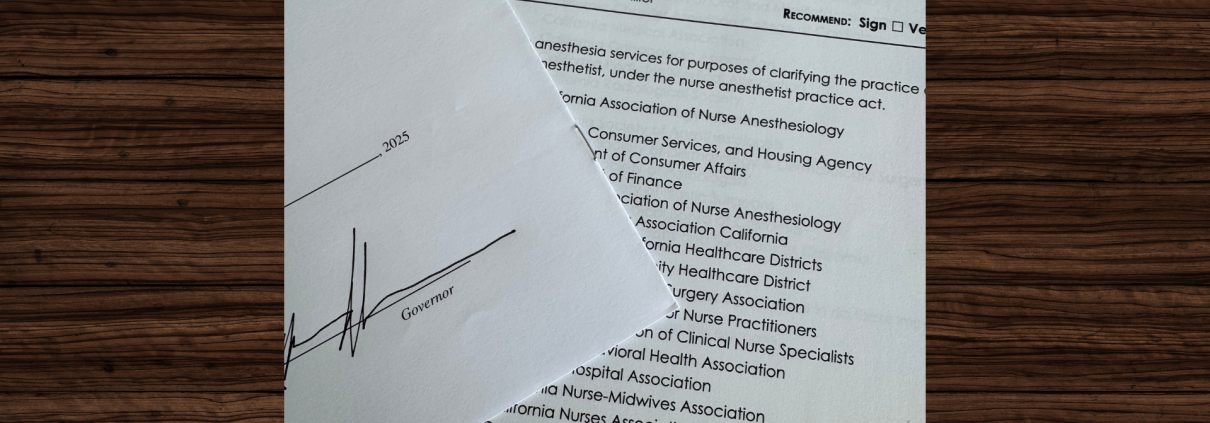
(SACRAMENTO, CA) –Today, Governor Gavin Newsom signed AB 876 (Flora) into law, reaffirming Certified Registered Nurse Anesthetists’ (CRNAs) essential role in the state’s health care system. The legislation codifies current, safe, and effective practices, ensuring CRNAs can continue delivering high-quality anesthesia care independently, thereby strengthening patient access, workforce stability, and health care equity.
“On behalf of my district and constituents, I’m thrilled Governor Newsom today signed AB 876 into law,” said Assembly Minority Leader Heath Flora (R-Ripon). “By clarifying CRNAs’ independent status and reinforcing the highest standards of anesthesia safety, Californians, particularly those living in rural and underserved regions of the state, will experience improved access to timely, high-quality, and cost-effective care.”
AB 876 amended existing statutes within the Nurse Anesthetist Act to clarify CRNAs’ longstanding independent authority in California. The bill protects Californians from unnecessary disruptions in care caused by regulatory uncertainty and ensures all facilities can provide accessible, efficient, and safe anesthesia services.
“We sincerely thank Governor Newsom and Assemblymember Flora for their leadership on this critical legislation,” said Emily Francke, CRNA, President, California Association of Nurse Anesthesiology. “We are proud to further our 40-year legacy of delivering safe, effective anesthesia services to all Californians — no matter their zip code.”
(SACRAMENTO, CA) –Today, Governor Gavin Newsom signed AB 876 (Flora) into law, reaffirming Certified Registered Nurse Anesthetists’ (CRNAs) essential role in the state’s health care system. The legislation codifies current, safe, and effective practices, ensuring CRNAs can continue delivering high-quality anesthesia care independently, thereby strengthening patient access, workforce stability, and health care equity.
“On behalf of my district and constituents, I’m thrilled Governor Newsom today signed AB 876 into law,” said Assembly Minority Leader Heath Flora (R-Ripon). “By clarifying CRNAs’ independent status and reinforcing the highest standards of anesthesia safety, Californians, particularly those living in rural and underserved regions of the state, will experience improved access to timely, high-quality, and cost-effective care.”
AB 876 amended existing statutes within the Nurse Anesthetist Act to clarify CRNAs’ longstanding independent authority in California. The bill protects Californians from unnecessary disruptions in care caused by regulatory uncertainty and ensures all facilities can provide accessible, efficient, and safe anesthesia services.
“We sincerely thank Governor Newsom and Assemblymember Flora for their leadership on this critical legislation,” said Emily Francke, CRNA, President, California Association of Nurse Anesthesiology. “We are proud to further our 40-year legacy of delivering safe, effective anesthesia services to all Californians — no matter their zip code.”
(SACRAMENTO, CA) – Today, Emily Francke, CRNA, President of the California Association of Nurse Anesthesiology (CANA), issued the following statement in response to the California Legislature passing AB 876 (Flora) with strong, bipartisan support:
“We are thankful and encouraged to see AB 876 continue its strong momentum. Throughout this process, California legislators have shown a deep understanding for the need to protect timely, high-quality anesthesia care for residents throughout the state. This bill ensures that Certified Registered Nurse Anesthetists / Anesthesiologists (CRNAs) can continue practicing to the full extent of their education and training, especially in underserved communities that depend on them most.
“We are also deeply appreciative of the broad coalition of labor organizations, provider associations, hospitals, and academic institutions that have stood with us in support of AB 876. The American Nurses Association California, California Hospital Association, California Nurses Association, California Ambulatory Surgery Association, United Nurses Association of California/Union of Health Care Professionals, California Association for Nurse Practitioners, National University School of Health Professions, Kaiser Permanente Nurse Anesthetists Association, and dozens of others have played a vital role in communicating the importance of this measure.
“When signed into law, AB 876 will deliver long-overdue clarity to existing statutes and reaffirm the essential role of CRNAs in California’s health care system. The bill does not expand CRNA scope, but rather codifies current, safe, and effective practices to prevent future misunderstandings.
“By closing care gaps and reinforcing the highest standards of anesthesia safety, AB 876 strengthens patient access, workforce stability, and health care equity. We commend Assemblymember Heath Flora (R-Ripon) and Senator Angelique Ashby (D-Sacramento) for their leadership and commitment to advancing this important legislation.
“On behalf of CRNAs – and Californians – statewide, we extend our sincerest gratitude to the California Legislature. As AB 876 moves to the Governor’s desk, CANA remains focused on protecting patient access, preventing unnecessary disruptions, and delivering the safe, effective anesthesia services Californians deserve.”
(SACRAMENTO, CA) – Today, Emily Francke, CRNA, President of the California Association of Nurse Anesthesiology (CANA), issued the following statement in response to the California Legislature passing AB 876 (Flora) with strong, bipartisan support:
“We are thankful and encouraged to see AB 876 continue its strong momentum. Throughout this process, California legislators have shown a deep understanding for the need to protect timely, high-quality anesthesia care for residents throughout the state. This bill ensures that Certified Registered Nurse Anesthetists / Anesthesiologists (CRNAs) can continue practicing to the full extent of their education and training, especially in underserved communities that depend on them most.
“We are also deeply appreciative of the broad coalition of labor organizations, provider associations, hospitals, and academic institutions that have stood with us in support of AB 876. The American Nurses Association California, California Hospital Association, California Nurses Association, California Ambulatory Surgery Association, United Nurses Association of California/Union of Health Care Professionals, California Association for Nurse Practitioners, National University School of Health Professions, Kaiser Permanente Nurse Anesthetists Association, and dozens of others have played a vital role in communicating the importance of this measure.
“When signed into law, AB 876 will deliver long-overdue clarity to existing statutes and reaffirm the essential role of CRNAs in California’s health care system. The bill does not expand CRNA scope, but rather codifies current, safe, and effective practices to prevent future misunderstandings.
“By closing care gaps and reinforcing the highest standards of anesthesia safety, AB 876 strengthens patient access, workforce stability, and health care equity. We commend Assemblymember Heath Flora (R-Ripon) and Senator Angelique Ashby (D-Sacramento) for their leadership and commitment to advancing this important legislation.
“On behalf of CRNAs – and Californians – statewide, we extend our sincerest gratitude to the California Legislature. As AB 876 moves to the Governor’s desk, CANA remains focused on protecting patient access, preventing unnecessary disruptions, and delivering the safe, effective anesthesia services Californians deserve.”
By Kuljit Sapraj, CRNA
Central California feeds the state and the nation. Yet too often, our region does not receive the same investment in health care that we give back in food, energy, and labor. Rural families deserve better.
As a Certified Registered Nurse Anesthetist (CRNA) practicing in Madera County, I know the challenges our communities face in accessing safe and timely care. When Madera Community Hospital reopened this year, it was a victory for our entire region — thanks to the leadership of Senator Anna Caballero, Assemblymember Esmeralda Soria, AAM, and many others who understood what was at stake. Their work ensured that over 150,000 residents once again have care close to home.
But our work is not finished. Rural California continues to face provider shortages, rising costs, and the very real threat of more closures. Adventist Health has already warned that two Central Valley hospitals are at risk. Across the nation, nearly one in five Americans lives in a “health care desert,” where services like maternity care, surgery, or anesthesia are simply unavailable. We cannot allow that to happen here.
That’s why AB 876 so important. Championed by Assemblymember Heath Flora, this bill is a lifeline for rural hospitals and their patients. AB 876 makes clear that CRNAs — highly trained anesthesia professionals — have long-standing authority to provide care independently. This clarity is critical for small hospitals and community clinics that operate on razor-thin margins and cannot afford duplicate roles, costly delays, or restrictive policies that take providers away from the bedside.
For decades, CRNAs have safely delivered anesthesia in every setting — from surgical centers and maternity wards to trauma bays — including in California counties where there is a reduction in physician anesthesiologists. We are trusted members of the health care team, committed to showing up day and night, rural or urban, wherever anesthesia is needed.
AB 876 empowers hospitals to use every available provider efficiently, keeping care affordable, timely, and local. For Central Valley families, this can mean the difference between receiving treatment in their own community or having to travel hours for surgery.
For the patients I serve in Madera County and across the Valley, the message is simple: AB 876 protects access to safe anesthesia services, prevents dangerous gaps in care, and ensures that no Californian is left behind because of their zip code.
Kuljit Sapraj is a Certified Registered Nurse Anesthetist (CRNA) with a doctoral degree in nurse anesthesia, serving patients at Madera Community Hospital.
By Kuljit Sapraj, CRNA
Central California feeds the state and the nation. Yet too often, our region does not receive the same investment in health care that we give back in food, energy, and labor. Rural families deserve better.
As a Certified Registered Nurse Anesthetist (CRNA) practicing in Madera County, I know the challenges our communities face in accessing safe and timely care. When Madera Community Hospital reopened this year, it was a victory for our entire region — thanks to the leadership of Senator Anna Caballero, Assemblymember Esmeralda Soria, AAM, and many others who understood what was at stake. Their work ensured that over 150,000 residents once again have care close to home.
But our work is not finished. Rural California continues to face provider shortages, rising costs, and the very real threat of more closures. Adventist Health has already warned that two Central Valley hospitals are at risk. Across the nation, nearly one in five Americans lives in a “health care desert,” where services like maternity care, surgery, or anesthesia are simply unavailable. We cannot allow that to happen here.
That’s why AB 876 so important. Championed by Assemblymember Heath Flora, this bill is a lifeline for rural hospitals and their patients. AB 876 makes clear that CRNAs — highly trained anesthesia professionals — have long-standing authority to provide care independently. This clarity is critical for small hospitals and community clinics that operate on razor-thin margins and cannot afford duplicate roles, costly delays, or restrictive policies that take providers away from the bedside.
For decades, CRNAs have safely delivered anesthesia in every setting — from surgical centers and maternity wards to trauma bays — including in California counties where there is a reduction in physician anesthesiologists. We are trusted members of the health care team, committed to showing up day and night, rural or urban, wherever anesthesia is needed.
AB 876 empowers hospitals to use every available provider efficiently, keeping care affordable, timely, and local. For Central Valley families, this can mean the difference between receiving treatment in their own community or having to travel hours for surgery.
For the patients I serve in Madera County and across the Valley, the message is simple: AB 876 protects access to safe anesthesia services, prevents dangerous gaps in care, and ensures that no Californian is left behind because of their zip code.
Kuljit Sapraj is a Certified Registered Nurse Anesthetist (CRNA) with a doctoral degree in nurse anesthesia, serving patients at Madera Community Hospital.
Rosemont, Ill. — The American Association of Nurse Anesthesiology (AANA) is pleased to announce CRNA Insight, created in partnership with the California Association of Nurse Anesthesiology (CANA) and designed to help Registered Nurses (RNs) and Advanced Practice Registered Nurses (APRNs) navigate the competitive admissions process to nurse anesthesiology programs.
Just last year, AANA launched a new RN-APRN membership category for skilled nurses who aspire to shift their professional focus towards the practice of anesthesia. CRNA Insight serves to guide AANA’s RN and APRN members through the often-challenging journey to CRNA school.
“AANA is committed to helping our more than 1200 RN-APRN members achieve their professional goals,” said Amy Sherwood, CAE, AANA’s Chief Membership Officer. “Through this product, we provide our members the tools, hands-on learning and networking to support a competitive edge and stand out as qualified CRNA candidates who are the future of this profession. This is an exciting time.”
CRNA Insight fills knowledge gaps in the admissions process, offering expert-led lessons and actionable strategies to boost RNs’ and APRNs’ success in a user-friendly, on-demand format. Backed by CRNA educators for accurate, relevant guidance, CRNA Insight includes targeted lessons on topics like pathophysiology and application preparation, practical strategies and insider insights from top CRNA/nurse anesthesiologist leaders, and exclusive content from experienced educators and program directors.
“CRNA Insight offers the optimal foundation for future CRNAs to learn the ins and out of what they need to succeed in the application process for nurse anesthesiology programs,” said Jacob Schonau-Taylor, CRNA, co-creator of CRNA Insight and a course instructor on the platform. “I’m incredibly proud of what CRNA Insight has become and excited for the meaningful educational impact it will have on AANA’s RN-APRN membership.”
CRNA Insight is now available on-demand at crnainsight.aana.com.
Rosemont, Ill. — The American Association of Nurse Anesthesiology (AANA) is pleased to announce CRNA Insight, created in partnership with the California Association of Nurse Anesthesiology (CANA) and designed to help Registered Nurses (RNs) and Advanced Practice Registered Nurses (APRNs) navigate the competitive admissions process to nurse anesthesiology programs.
Just last year, AANA launched a new RN-APRN membership category for skilled nurses who aspire to shift their professional focus towards the practice of anesthesia. CRNA Insight serves to guide AANA’s RN and APRN members through the often-challenging journey to CRNA school.
“AANA is committed to helping our more than 1200 RN-APRN members achieve their professional goals,” said Amy Sherwood, CAE, AANA’s Chief Membership Officer. “Through this product, we provide our members the tools, hands-on learning and networking to support a competitive edge and stand out as qualified CRNA candidates who are the future of this profession. This is an exciting time.”
CRNA Insight fills knowledge gaps in the admissions process, offering expert-led lessons and actionable strategies to boost RNs’ and APRNs’ success in a user-friendly, on-demand format. Backed by CRNA educators for accurate, relevant guidance, CRNA Insight includes targeted lessons on topics like pathophysiology and application preparation, practical strategies and insider insights from top CRNA/nurse anesthesiologist leaders, and exclusive content from experienced educators and program directors.
“CRNA Insight offers the optimal foundation for future CRNAs to learn the ins and out of what they need to succeed in the application process for nurse anesthesiology programs,” said Jacob Schonau-Taylor, CRNA, co-creator of CRNA Insight and a course instructor on the platform. “I’m incredibly proud of what CRNA Insight has become and excited for the meaningful educational impact it will have on AANA’s RN-APRN membership.”
CRNA Insight is now available on-demand at crnainsight.aana.com.
(SACRAMENTO, CA) – Today, Emily Francke, CRNA, President of the California Association of Nurse Anesthesiology (CANA), issued the following statement in response to the California Assembly Committee on Business and Professions passing AB 876 by Assemblymember Heath Flora (R-Ripon) on a vote of 15-1:
“We are thankful and encouraged by yesterday’s vote in the Assembly Business and Professions Committee to advance AB 876—a critical step toward protecting timely, high-quality anesthesia care for Californians across the state. This bill ensures that Certified Registered Nurse Anesthetists / Anesthesiologists (CRNAs) can continue practicing to the full extent of their education and training, especially in communities that depend on them most.
“We are also deeply appreciative of the Committee members and consultants for their tireless advocacy regarding this bill, in addition to the many professional organizations who stood with us today in support. Representatives from the American Nurses Association California, California Behavioral Health Association, California Nurses Association, United Nurses Association of California / Union of Health Care Professionals, Samuel Merritt University, and National University School of Health Professions, including dozens of others, all voiced support for this bill.
“It’s important to underscore that AB 876 is not controversial. It brings long-overdue clarity to existing statutes and reaffirms the vital role of CRNAs in California’s health care system. This bill does not expand scope—it codifies current, safe, and effective practices to prevent future misunderstandings, like the incident that occurred in Modesto last year that led to nearly 1000 surgeries to be cancelled—heavily impacting Medicare and Medi-Cal patients.
“AB 876 ensures that care gaps are closed while maintaining the highest standards of anesthesia care from trained experts. We commend Assemblymember Flora for his leadership and thank the Committee members for recognizing the urgency of this issue. Their support demonstrates a shared commitment to patient safety, workforce stability, and equitable access to care.
“On behalf of CRNAs statewide, we remain focused on protecting patient access, preventing unnecessary disruptions, and delivering the safe, effective anesthesia services Californians deserve.”
AB 876 now advances to the Assembly Appropriations Committee.
About California Association of Nurse Anesthesiology (CANA)
CANA represents CRNAs across the state. Since 1931, CANA has provided leadership, advocacy, and education to advance patient safety and support the nurse anesthesia profession. Learn more at www.canainc.org.
(SACRAMENTO, CA) – Today, Emily Francke, CRNA, President of the California Association of Nurse Anesthesiology (CANA), issued the following statement in response to the California Assembly Committee on Business and Professions passing AB 876 by Assemblymember Heath Flora (R-Ripon) on a vote of 15-1:
“We are thankful and encouraged by yesterday’s vote in the Assembly Business and Professions Committee to advance AB 876—a critical step toward protecting timely, high-quality anesthesia care for Californians across the state. This bill ensures that Certified Registered Nurse Anesthetists / Anesthesiologists (CRNAs) can continue practicing to the full extent of their education and training, especially in communities that depend on them most.
“We are also deeply appreciative of the Committee members and consultants for their tireless advocacy regarding this bill, in addition to the many professional organizations who stood with us today in support. Representatives from the American Nurses Association California, California Behavioral Health Association, California Nurses Association, United Nurses Association of California / Union of Health Care Professionals, Samuel Merritt University, and National University School of Health Professions, including dozens of others, all voiced support for this bill.
“It’s important to underscore that AB 876 is not controversial. It brings long-overdue clarity to existing statutes and reaffirms the vital role of CRNAs in California’s health care system. This bill does not expand scope—it codifies current, safe, and effective practices to prevent future misunderstandings, like the incident that occurred in Modesto last year that led to nearly 1000 surgeries to be cancelled—heavily impacting Medicare and Medi-Cal patients.
“AB 876 ensures that care gaps are closed while maintaining the highest standards of anesthesia care from trained experts. We commend Assemblymember Flora for his leadership and thank the Committee members for recognizing the urgency of this issue. Their support demonstrates a shared commitment to patient safety, workforce stability, and equitable access to care.
“On behalf of CRNAs statewide, we remain focused on protecting patient access, preventing unnecessary disruptions, and delivering the safe, effective anesthesia services Californians deserve.”
AB 876 now advances to the Assembly Appropriations Committee.
About California Association of Nurse Anesthesiology (CANA)
CANA represents CRNAs across the state. Since 1931, CANA has provided leadership, advocacy, and education to advance patient safety and support the nurse anesthesia profession. Learn more at www.canainc.org.
(SACRAMENTO, CA) – Today, the California Association of Nurse Anesthesiology (CANA) announced support for its sponsored bill AB 876 by Assemblymember Heath Flora (R-Ripon) from the California Nurses Association / National Nurses United, United Nurses Association of California / Union of Health Care Professionals, and Kaiser Permanente Nurse Anesthetists Association.
“We’re grateful for our colleagues at CNA, UNAC/UHCP, and KPNAA for understanding the urgent need for AB 876. California CRNAs have provided anesthesia services without physician supervision for nearly 40 years, ensuring Californians throughout the state, particularly in rural and underserved regions, receive timely, high-quality, and cost-effective care,” said Emily Francke, CRNA, President, CANA. “With Assemblymember Flora’s leadership and broad support from allied professions, stakeholders, and the California Board of Registered Nursing, AB 876 should be passed out of the Legislature and signed by Governor Newsom as soon as possible.”
When signed into law, AB 876 (Flora) will make it abundantly clear for legislators, policymakers, and hospital administrators that Certified Registered Nurse Anesthetists (CRNAs), or nurse anesthesiologists, are authorized to provide anesthesia care independently. Specifically, the bill clarifies existing statutes within the Nurse Anesthetist Act to safeguard patients’ access to quality and timely anesthesia care and improve health outcomes.
“We are committed to building a better workplace and a healthier world, which is why we support AB 876,” said Daniel Bell, DNP, CRNA, United Nurses Association of California (UNAC) / Union of Health Care Professionals (UHCP). “By passing this measure, legislators will have taken decisive action to address provider redundancies that contribute to the state’s current anesthesia staffing crisis while preventing costly disruptions in care.”
AB 876 does not expand CRNAs’ scope of practice, nor does it change how CRNAs currently provide anesthesia in the state. The bill maintains that CRNAs have long provided anesthesia services without physician supervision, in line with regulatory opinions from the 1980s, case law, and California’s 2009 federal opt-out decision. In the operating room, it’s up to each health care facility to determine how they provide anesthesia services to patients. They can use a CRNA-only model; a collaborative model where CRNAs and physician anesthesiologists work together, but independently; or a physician anesthesiologist-led model.
Despite CRNAs’ longstanding independence, special interests are purposefully exploiting misinterpretations of state statute to challenge CRNAs’ established practice, place an undue burden on facility administrators, risk patient safety, and undermine patient access to timely and affordable anesthesia care.
“For decades, California CRNAs have been at the forefront of providing anesthesia services. It’s time for special interests to stop putting patients in the middle of political fights and instead work together on behalf of the Californians that entrust us with their lives,” said Kathleen Theobald, Executive Director, Kaiser Permanente Nurse Anesthetists Association (KPNAA). “We’re grateful to CANA for sponsoring this measure and Assemblymember Flora for championing this issue on behalf of his constituents and Californians throughout the state who rely on timely and affordable access to high-quality anesthesia care.”
By putting all statutes and codes in one place, AB 876 will avoid confusion, protect patient access, and prevent costly, unnecessary disruptions in anesthesia care and services. CRNAs are anesthesia experts. They must earn a BSN (or equivalent degree), obtain an RN license, complete a doctoral anesthesia program (DNP or DNAP), and nearly 10,000 hours of clinical and ICU training before taking the national certification exam. Unlike physician anesthesiologists, CRNAs must be board-certified to provide anesthesia services, with re-certifications required every 4 years.
AB 876 is set to be heard on April 22 in the Assembly Business and Professions Committee.
About California Association of Nurse Anesthesiology (CANA)
CANA represents CRNAs across the state. Since 1931, CANA has provided leadership, advocacy, and education to advance patient safety and support the nurse anesthesia profession. Learn more at www.canainc.org.
(SACRAMENTO, CA) – Today, the California Association of Nurse Anesthesiology (CANA) announced support for its sponsored bill AB 876 by Assemblymember Heath Flora (R-Ripon) from the California Nurses Association / National Nurses United, United Nurses Association of California / Union of Health Care Professionals, and Kaiser Permanente Nurse Anesthetists Association.
“We’re grateful for our colleagues at CNA, UNAC/UHCP, and KPNAA for understanding the urgent need for AB 876. California CRNAs have provided anesthesia services without physician supervision for nearly 40 years, ensuring Californians throughout the state, particularly in rural and underserved regions, receive timely, high-quality, and cost-effective care,” said Emily Francke, CRNA, President, CANA. “With Assemblymember Flora’s leadership and broad support from allied professions, stakeholders, and the California Board of Registered Nursing, AB 876 should be passed out of the Legislature and signed by Governor Newsom as soon as possible.”
When signed into law, AB 876 (Flora) will make it abundantly clear for legislators, policymakers, and hospital administrators that Certified Registered Nurse Anesthetists (CRNAs), or nurse anesthesiologists, are authorized to provide anesthesia care independently. Specifically, the bill clarifies existing statutes within the Nurse Anesthetist Act to safeguard patients’ access to quality and timely anesthesia care and improve health outcomes.
“We are committed to building a better workplace and a healthier world, which is why we support AB 876,” said Daniel Bell, DNP, CRNA, United Nurses Association of California (UNAC) / Union of Health Care Professionals (UHCP). “By passing this measure, legislators will have taken decisive action to address provider redundancies that contribute to the state’s current anesthesia staffing crisis while preventing costly disruptions in care.”
AB 876 does not expand CRNAs’ scope of practice, nor does it change how CRNAs currently provide anesthesia in the state. The bill maintains that CRNAs have long provided anesthesia services without physician supervision, in line with regulatory opinions from the 1980s, case law, and California’s 2009 federal opt-out decision. In the operating room, it’s up to each health care facility to determine how they provide anesthesia services to patients. They can use a CRNA-only model; a collaborative model where CRNAs and physician anesthesiologists work together, but independently; or a physician anesthesiologist-led model.
Despite CRNAs’ longstanding independence, special interests are purposefully exploiting misinterpretations of state statute to challenge CRNAs’ established practice, place an undue burden on facility administrators, risk patient safety, and undermine patient access to timely and affordable anesthesia care.
“For decades, California CRNAs have been at the forefront of providing anesthesia services. It’s time for special interests to stop putting patients in the middle of political fights and instead work together on behalf of the Californians that entrust us with their lives,” said Kathleen Theobald, Executive Director, Kaiser Permanente Nurse Anesthetists Association (KPNAA). “We’re grateful to CANA for sponsoring this measure and Assemblymember Flora for championing this issue on behalf of his constituents and Californians throughout the state who rely on timely and affordable access to high-quality anesthesia care.”
By putting all statutes and codes in one place, AB 876 will avoid confusion, protect patient access, and prevent costly, unnecessary disruptions in anesthesia care and services. CRNAs are anesthesia experts. They must earn a BSN (or equivalent degree), obtain an RN license, complete a doctoral anesthesia program (DNP or DNAP), and nearly 10,000 hours of clinical and ICU training before taking the national certification exam. Unlike physician anesthesiologists, CRNAs must be board-certified to provide anesthesia services, with re-certifications required every 4 years.
AB 876 is set to be heard on April 22 in the Assembly Business and Professions Committee.
About California Association of Nurse Anesthesiology (CANA)
CANA represents CRNAs across the state. Since 1931, CANA has provided leadership, advocacy, and education to advance patient safety and support the nurse anesthesia profession. Learn more at www.canainc.org.
(Sacramento, CA)—California Association of Nurse Anesthesiology (CANA) President Emily Francke, CRNA today issued the following statement commending the California Board of Registered Nursing (BRN) for their unanimous vote in support of AB 876 (Flora) during their board meeting on March 20, 2025:
“AB 876 makes it abundantly clear how critical a role Certified Registered Nurse Anesthetists / Anesthesiologists (CRNAs) play in California. The BRN’s unanimous support for this crucial piece of legislation underscores their commitment to patient safety and strengthening California’s anesthesia workforce.
“Despite our longstanding independence, special interests are purposefully exploiting misinterpretations of state statute to challenge CRNAs’ established practice, risk patient safety, and undermine patient access to timely and affordable anesthesia care. By providing legislative clarity and codifying existing statutes in one place, AB 876 will help avoid confusion, protect patient access, and prevent costly and unnecessary disruptions in anesthesia care.
“CANA remains dedicated to advocating for policies that safeguard the ability of CRNAs to practice to the full extent of their education and training. Ahead of the March 20 meeting, more than 200 CRNAs contacted the BRN to ensure they understood the urgency and critical importance of this legislation. Together, under the umbrella of CANA, California CRNAs will remain focused on expanding access to anesthesia care while ensuring that patients receive the highest quality of care possible.”
(Sacramento, CA)—California Association of Nurse Anesthesiology (CANA) President Emily Francke, CRNA today issued the following statement commending the California Board of Registered Nursing (BRN) for their unanimous vote in support of AB 876 (Flora) during their board meeting on March 20, 2025:
“AB 876 makes it abundantly clear how critical a role Certified Registered Nurse Anesthetists / Anesthesiologists (CRNAs) play in California. The BRN’s unanimous support for this crucial piece of legislation underscores their commitment to patient safety and strengthening California’s anesthesia workforce.
“Despite our longstanding independence, special interests are purposefully exploiting misinterpretations of state statute to challenge CRNAs’ established practice, risk patient safety, and undermine patient access to timely and affordable anesthesia care. By providing legislative clarity and codifying existing statutes in one place, AB 876 will help avoid confusion, protect patient access, and prevent costly and unnecessary disruptions in anesthesia care.
“CANA remains dedicated to advocating for policies that safeguard the ability of CRNAs to practice to the full extent of their education and training. Ahead of the March 20 meeting, more than 200 CRNAs contacted the BRN to ensure they understood the urgency and critical importance of this legislation. Together, under the umbrella of CANA, California CRNAs will remain focused on expanding access to anesthesia care while ensuring that patients receive the highest quality of care possible.”
On March 11, 2025, CANA made history with our most successful and well-attended Lobby Day to date. CRNAs and nurse anesthesia residents from across the state gathered in Sacramento, demonstrating the strength of our profession and our unwavering commitment to the patients we serve.
We began the day by hearing from Assemblymember Heath Flora (R-Ripon), a steadfast advocate for protecting Californians’ ability to access timely and affordable anesthesia care. Assemblymember Flora’s dedication to our profession was made clear in his energizing and motivating remarks about his California Anesthesia Access Package (AB 876 and AB 1215), which helped set the tone for a powerful day of advocacy.
If you attended, you know that we hit the ground running, meeting with lawmakers and their staff to illustrate the essential role CRNAs play in California’s health care landscape. CANA members shared firsthand experiences of delivering care in rural communities, labor and delivery suites, military settings, and underserved areas—highlighting the direct impact CRNAs have on patient access to safe, cost-effective anesthesia care.
Members were also equipped with the following handouts:
- Fast Facts re: California Anesthesia Access Package (AB 876 & AB 1215) – These bills codify existing statutes in one place to help prevent misinterpretations that continue to be exploited by special interests, which disrupts patient care and drives up health care costs.
- Title 22 Reform – Timeline showing CANA’s 30+ years of advocacy to modernize outdated regulations that have led to confusion, unnecessary restrictions in hospitals, and barriers to care.
- CRNAs as Key Players in Addressing California’s Opioid Crisis – Highlighted CRNAs’ expertise related to opioid-sparing anesthesia techniques and interventional pain management, reinforcing our role in reducing opioid exposure and improving patient outcomes.
Throughout the day CANA underscored that our advocacy is not just about our profession—it’s about ensuring every patient in California, regardless of location, has access to safe, high-quality anesthesia care; using the story of how the California Department of Public Health’s unjustified actions last year negatively impacted thousands of Medi-Cal and Medicare beneficiaries as an example, we made it clear that this issue cannot be ignored.
The response was overwhelmingly supportive.
Legislators and staff recognized the urgency of our priority issues, reinforcing that this effort is not just about CRNAs—it’s about doing what is right for California patients.
Thank you to everyone who attended any and all Lobby Day events, including those who ended the day with us at Smic’s for our CANA-hosted PAC networking reception.
Your voice matters, and your advocacy has an impact far beyond what you can see. With more than 3,000 CRNAs in California and growing, our strength lies in unity. One voice, one mission. Let’s keep this impressive momentum going.